Glaucoma & Ocular Hypertension
Glaucoma affects over 70 million people worldwide and over 12 million in the EU alone. Risk of glaucoma is higher for people suffering from diabetes, hypertension and the elderly as well as for specific ethnic backgrounds. Glaucoma’s effect on society is especially impactful in ageing societies like EU and USA, where the number of affected people increases steadily. It is a chronic condition with no permanent cure and is the second leading cause of blindness. Glaucoma decreases the quality of life of the patients affecting their social life and independence. It causes significant workforce loss and creates a heavy economic burden on social systems and. 50% of the affected people are not aware that they are suffering from glaucoma. The most prominent and stealthy form of it, namely open-angle glaucoma, is mainly caused by chronic ocular hypertension.
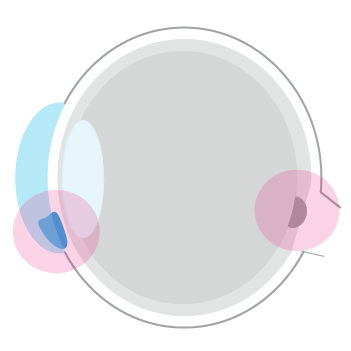
Ocular hypertension is the physiological condition of elevated intraocular pressure (IOP). The ciliary body in the posterior chamber of the eye produces the fluid “aqueous humour.” The produced aqueous humour is drained through the trabecular meshwork into the bloodstream. If the drainage through the trabecular meshwork cannot keep up with the aqueous humour production, IOP starts to increase. As the most prominent risk factor of open-angle glaucoma, ocular hypertension is observable with regular measurements of intraocular pressure (IOP). The presence of ocular hypertension (high IOP) over extended periods predominantly leads to optic nerve damage and permanent loss of vision in some cases (glaucoma).
Conventional IOP Measurement and the Trouble Within
Glaucoma management relies heavily on IOP measurements and their accuracy. Conventional methods used to diagnose high IOP, monitor the progression of glaucoma and create treatment algorithms depend on a single IOP measurement conducted at the clinic with a tonometer. However, single point IOP measurement leads to decreased diagnostic accuracy and limited therapeutic success because:
- the IOP displays circadian change, and a majority of patients have lower daytime IOP values, and
- conventional measurement methods can only be used during working hours at the clinic. Therefore, single point measurement exposes patients to unnecessary risks and imposes a substantial financial burden on healthcare systems worldwide.
The ability to monitor IOP fluctuations over an extended period would allow doctors to formulate an earlier and more accurate diagnosis and would allow for the personalisation of drug and surgical therapeutic options.
The Importance of Diurnal IOP Fluctuation
Glaucoma, changes in the intraocular pressure, is an irreversible, chronic and progressive disease that causes visual field loss and destruction of retinal ganglion cells. It is the leading cause of irreversible blindness worldwide (1) and among eye diseases, glaucoma is the second leading cause for blindness after cataracts (2). It is characterized by both functional […]
Glaucoma – Challenge and Solution
Glaucoma affects over 70 million people worldwide and over 12 million in the EU alone. Risk of glaucoma is higher for people suffering from diabetes, hypertension and the elderly as well as for specific ethnic backgrounds. It is a chronic condition with no permanent cure and is the second leading cause of blindness. 50% of […]
